In this comprehensive guide, you will learn everything you need to know about the pelvic floor from our experts at Pazona MD Urology in Nashville. Our dedicated team of urologists and providers help a lot of patients with pelvic floor dysfunction. Now it’s time you get the help you deserve, so let’s dive in.
What is the pelvic floor?
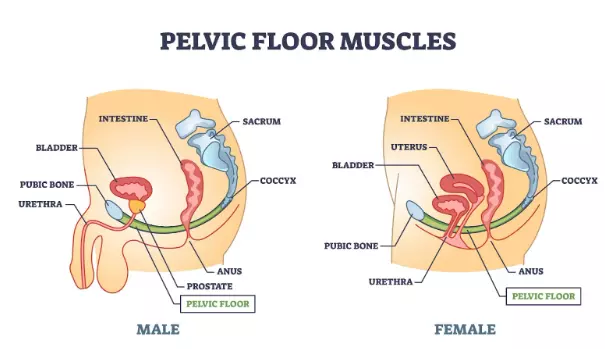
The pelvic floor is a complex network of muscles, ligaments, and tissues located at the base of the pelvis. These muscles form a sling or hammock that supports the bladder, rectum, and in women, the uterus and vagina. The pelvic floor muscles play a crucial role in maintaining continence, supporting pelvic organs, and contributing to sexual function.
When you have to urinate or have a bowel movement, the pelvic floor is relaxing. When you’re trying to hold in your “pee,” the pelvic floor muscles are now tightening. All those pleasurable muscle contractions during orgasm are coming from your pelvic floor muscles.
But the pelvic muscles are also so much more. They work in concert with your lower abdominal and back muscles to form your “core.” Whether you’re standing, walking, or lifting weights, you are engaging your pelvic floor muscles.
The pelvic floor even works with your diaphragm (internal muscle near your lungs that moves with breathing). Together with the other “core” muscles, they all control pressure inside your abdomen.
In other words, the pelvic floor is not a single muscle with a single function. It's a number of muscles and ligaments that perform sophisticated roles during every second of your life. Pretty cool stuff isn’t it?!
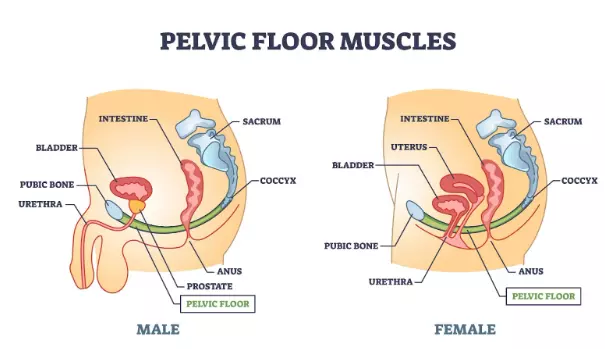
Where are the pelvic floor muscles located?
You’re sitting on your pelvic floor right now! The pelvic floor muscles are located on the bottom of your pelvis. Think about the whole area from:
- Below your pubic bone to …
- In from of your tailbone (coccyx) which is …
- Spanning from sit bone to sit bone (ischial tuberosities).
If you think about all of the deeper soft tissue around your anus, urethra and vagina (if you have one), then you're focusing on your pelvic floor muscles.
What is the anatomy of the pelvic floor muscles?
Either you’re still confused or you’re an anatomy geek like us. Both are ok.
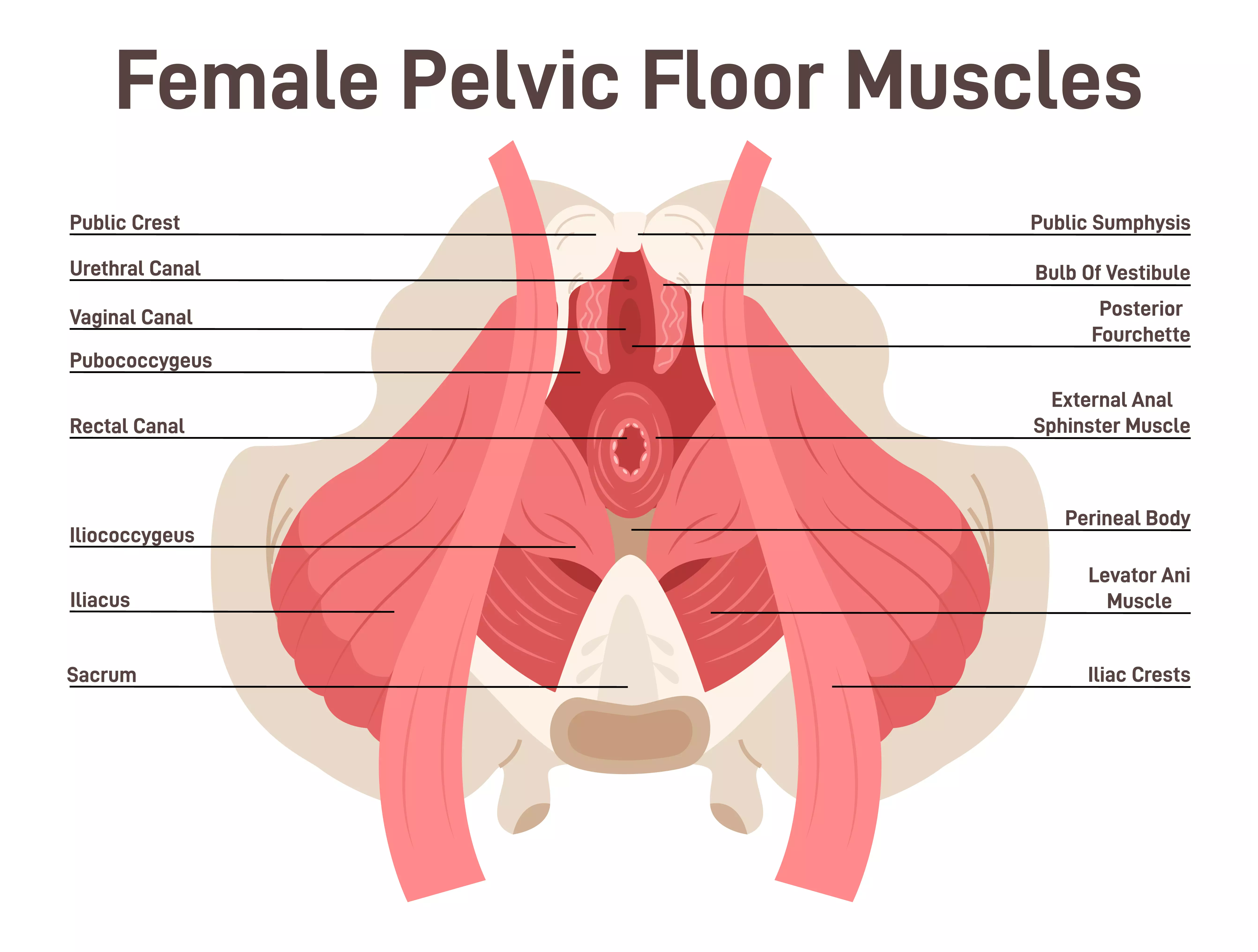
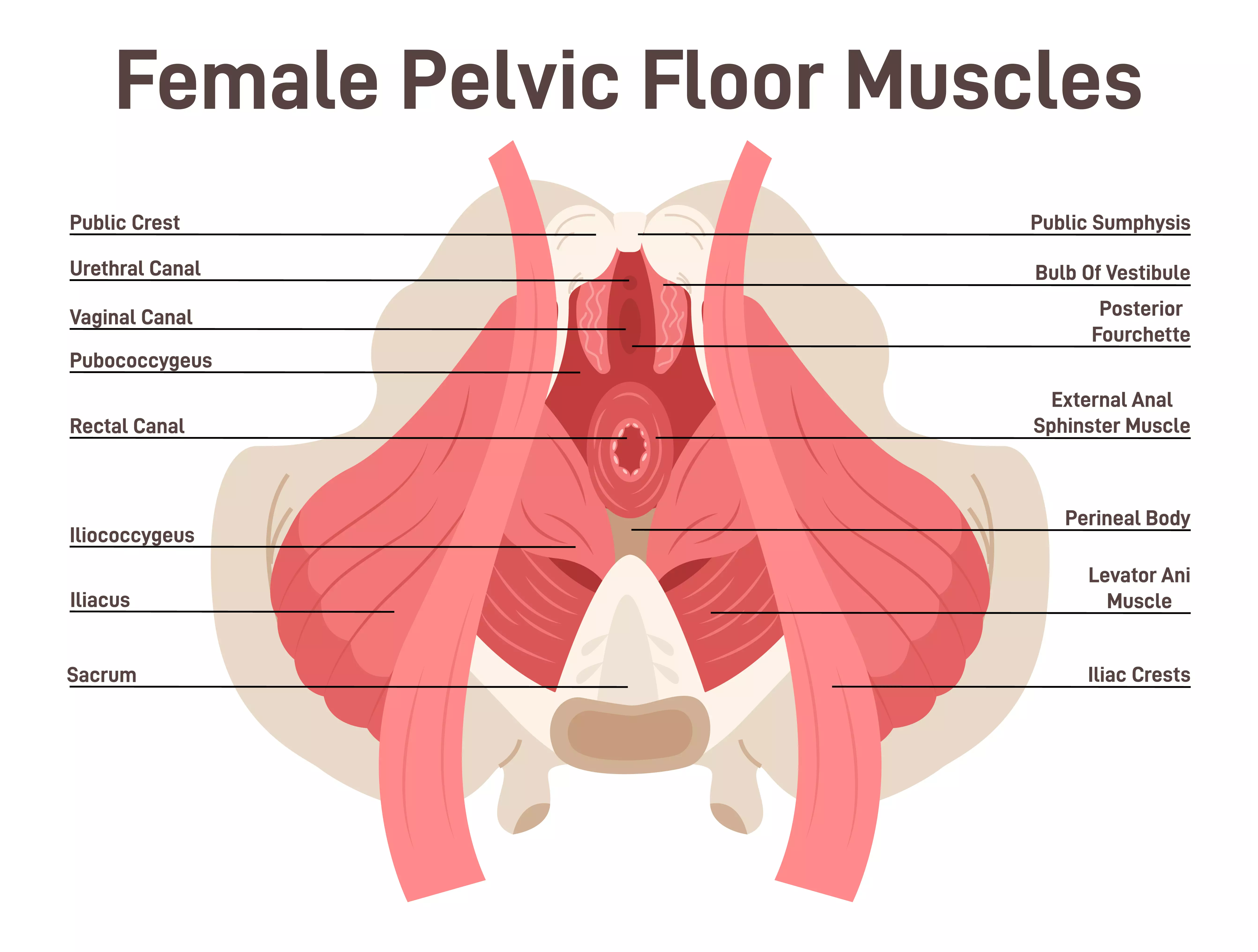
To get specific, the pelvic floor is comprised of several muscles, including the:
- Levator ani group (pubococcygeus, puborectalis, and iliococcygeus)
- Coccygeus muscle
These muscles work together to support the pelvic organs and maintain proper function. Take a look at the pelvic floor muscles in a biological female:
What do the pelvic floor muscles do?
Pelvic floor muscles are essential for:
- Controlling the release of urine and feces
- Holding the female internal pelvic organs in place (vagine, uterus)
- Sexual health (remember they squeeze during orgasm)
- Stabilizing the "core" during activities like walking, running, and lifting
So what happens when the pelvic floor muscles are not working properly? We thought you’d never ask!
Pelvic Floor Dysfunction
What is Pelvic Floor Dysfunction?
Pelvic floor dysfunction occurs when the pelvic floor muscles are too weak, too tight, or there is an imbalance in their function. This condition can lead to a variety of symptoms, affecting both men and women, although it is more common in women.
Pelvic floor dysfunction is arguably the most underdiagnosed and misunderstood medical disorder that we see as urology experts at Pazona MD Urology.
Women suffering with constipation or painful intercourse are often told, “there’s nothing we can do.” Women with incontinence are often rushed to surgery before trying pelvic floor exercises. Even men are often misdiagnosed with prostatitis or epididymitis (testicular pain) when the real source of their trouble is pelvic floor dysfunction.
What are the symptoms of pelvic floor dysfunction?
The symptoms of pelvic floor dysfunction vary depending on whether they are too tight, too loose, or just plain not working right.
Some of the more common symptoms of pelvic dysfunction include:
- Urinary incontinence (leakage of urine)
- Fecal incontinence (leakage of stool)
- Pelvic pain or pressure (e.g. testicle, prostate, or vaginal pain)
- Pain during intercourse
- Difficulty with bowel movements
- Lower back pain
How do I know if I have pelvic floor dysfunction?
It always starts with seeing a physician or provider with expertise in the pelvic floor. This means seeing a urologist or gynecologist that listens to you. A detailed history will often suggest that the pelvic floor is the source of your troubles.
We often find that pelvic pain in men and women varies in location, severity, and frequency, and is often due to pelvic floor dysfunction. Patients with underlying low back pain and obesity seem to have more pelvic floor issues as well.
Next, a thorough physical exam can typically identify pelvic floor dysfunction. Pelvic floor dysfunction usually doesn’t have any swelling or masses associated with it. This means ruling out hernias, scrotal, prostate or vaginal masses.
In men, a tight pelvic floor can present with tenderness in the perineum or above the testicle into the groin area. Women will often report tenderness or tightness on their pelvic exam.
A loose pelvic floor, almost exclusively seen in women, will demonstrate a hypermobile urethra with leakage of urine when the woman coughs. She may also have pelvic organ prolapse or bulging of the bladder/intestines/uterus out of the vaginal opening.
If necessary, a skilled expert in pelvic floor dysfunction will perform a comprehensive pelvic floor assessment, which measures the various components of pelvic floor muscle contractility. This includes pelvic floor muscle power, endurance, and speed to name a few.
What tests can diagnose pelvic floor dysfunction?
In most cases, a thorough history and physical examination can diagnose pelvic floor dysfunction. However, in select cases, neuromuscular testing (biofeedback) may be performed to further pinpoint the exact cause of the pelvic floor dysfunction.
Urodynamics
When women present with urinary incontinence, or involuntary leakage of urine, further diagnostic testing can be helpful to determine the underlying cause. With urodynamics, a small catheter is inserted into the urethra and rectum while fluid is slowly instilled into the bladder.
How the bladder and pelvic floor react to bladder filling and emptying can unmask pelvic floor dysfunction. Live x rays during urodynamics (video urodynamics) can suggest pelvic floor tightness or laxity (looseness).
Defecography
When your issues are more related to bowel movements, then an imaging test with x rays or MRI may be performed. Defecography involves filling your rectum with a barium paste and then taking pictures while you defecate to look at the pelvic floor muscles. Remember that the pelvic floor must relax in order to have a bowel movement. This test can help identify pelvic floor dysfunction as a cause of your constipation.
What are the causes of pelvic floor dysfunction?
Any condition that causes undue stress to the pelvic floor can lead to pelvic floor dysfunction. This includes:
- Childbirth
- Surgery
- Aging
- Obesity
- Chronic coughing
- Heavy lifting
- High-impact exercise
In women, it’s important to note that estrogen plays a vital role in the health of the pelvic floor. Post-menopausal women who are not using estrogen (systemic or vaginal) tend to have more pelvic floor dysfunction.
Pelvic Floor Therapy
What Is Pelvic Floor Therapy?
Pelvic floor therapy is a specialized form of physical therapy focused on strengthening and/or rehabilitating the pelvic floor muscles. It is an effective treatment for various pelvic floor disorders, including incontinence, pelvic pain, and prolapse.
Pelvic floor physical therapy is a non-surgical approach to treating pelvic floor dysfunction. It involves a thorough evaluation and personalized treatment plan by a trained physical therapist specializing in pelvic health.
What Are the Benefits of Pelvic Floor Therapy?
Depending on the symptoms of your pelvic floor dysfunction, pelvic floor therapy may lead to:
- Improved bladder and bowel control
- Reduced pelvic pain
- Enhanced sexual function
- Prevention or improvement of pelvic organ prolapse
- Better core stability
Like any therapy, consistency and focus are the key. Seeing a pelvic physical therapist on a regular basis can ensure you receive the most benefit from pelvic floor therapy.
Who Can Benefit from Pelvic Floor Physical Therapy?
Anyone searching for relief from the symptoms of pelvic floor dysfunction can benefit from pelvic floor physical therapy. However, their are select groups who should almost certainly consider seeing a pelvic floor physical therapist:
- Postpartum women
- Individuals with urinary or fecal incontinence
- Male and female patients with chronic pelvic pain
- Individuals with pelvic organ prolapse
- Men pre and post prostatectomy for prostate cancer (prevent or treat urinary leakage)
- Athletes with pelvic pain
What Can I Expect During Pelvic Floor Physical Therapy?
Although we will present some DIY pelvic floor exercises, we highly recommend that you seek out an experienced pelvic floor physical therapist to get you started on your exercise regimen.
You don’t want to perform strengthening pelvic floor exercises if your pelvic floor is already too tight. Also, unlike other muscle groups, it’s more difficult to determine if you are performing pelvic floor exercises correctly. These aren’t bicep curls where you can easily see the muscle contracting and relaxing.
Here’s what you can expect from pelvic floor therapy:
- Initial Assessment: A comprehensive evaluation of the patient’s medical history, symptoms, and pelvic floor function.
- Treatment Plan: A customized plan that may include exercises, manual therapy, biofeedback, and education.
- Follow-up Sessions: Regular sessions to monitor progress, adjust the treatment plan, and ensure the effectiveness of therapy.
What Techniques Are Used in Pelvic Floor Therapy?
Not all pelvic floor therapy is the same. Similar to trainers at the gym, a pelvic physical therapist may utilize a variety of techniques to improve your pelvic floor dysfunction:
- Biofeedback: A technique that uses sensors and computer feedback to help patients learn to control pelvic floor muscles.
- Manual Therapy: Hands-on techniques to massage and stretch the muscles and tissues.
- Pelvic Floor Exercises: Specific exercises designed to strengthen and relax the pelvic floor muscles.
- Electrical Stimulation: Using mild electrical currents to stimulate and strengthen pelvic floor muscles.
- Behavioral Training: Education on bladder and bowel habits, fluid and dietary management.
Pelvic Floor Exercises
Why Are Pelvic Floor Exercises Important?
Pelvic floor exercises are crucial for maintaining and improving the strength and function of the pelvic floor muscles. These exercises can prevent and treat pelvic floor dysfunction, enhance core stability, and improve overall quality of life.
Think about the amount of time some of us exercise all the other muscles in our body. And yet we ignore the pelvic floor muscles that control our ability to urinate, have bowel movements, and enjoy sexual activity. Doesn’t make sense does it?
Let’s explore the different types of pelvic floor exercises so we can truly engage in total body workouts moving forward.
What are the Best Types of Pelvic Floor Exercises?
Are pelvic floor muscles the same as Kegels? Yes but they are so much more as well. Kegels are only one type of pelvic floor exercise.
So how do you tighten your pelvic floor muscles? What muscles do you squeeze for the pelvic floor? We’ve got you covered.
Ask any trainer or gym junkie, “what are the best exercises for . . . “ and you’re likely to get 100 different answers. In researching the best pelvic floor exercises, there are some consistent choices amongst the experts. Here are the top 3 pelvic floor exercises:
Kegel Exercises
Kegels are the gold standard for strengthening the pelvic floor muscles. Why? Because you are isolating the actual pelvic floor muscles (levator ani and coccygeus) to build strength. We'll describe how to perform Kegel exercises shortly.
Bridge
Also known as a “glute bridge” or the “bridge pose” for the yoga fans, this is an easy exercise to perform. Lay down on your back with your knees bent and your feet flat on the floor. Lift your hips upwards while maintaining floor contact with your feet, arms, upper back, neck and head. Hold your hips up by pushing through your feet and squeezing your butt and hamstrings.
The bridge engages the pelvic floor, core, and posterior leg muscles. Hold the pose for at least 10 seconds and repeat for 10 repetitions.
Squats
Squats are a great lower body and core exercise in addition to strengthening the pelvic floor muscles. The best part is that you don’t need to load up the barbell with 300 lbs to strengthen your pelvic floor muscles. Most people “know” how to perform a squat, however, most people perform them incorrectly. Here are the keys to doing an effective squat for your pelvic floor muscles:
- Stand a little wider than shoulder width with your toes pointed slightly outward.
- SLOWLY (it should take 3-4 seconds) lower your body down while keeping your back and chest upright. If you are bending at the hips this is not a squat, it’s a hip hinge.
- Lower yourself until your knees are at 90 degrees or you feel limited mobility.
- Push yourself back up over 1 second.
- Repeat 10-15 times.
Let’s spend a little more time on Kegels. Why? Well when properly performed, Kegels are isolating the levator ani and coccygeus muscles. The proper muscles of the pelvic floor. As a man you’ve probably intentionally “worked out” these muscles zero times. As a woman, there’s a good chance you weren’t doing them properly.
Here’s a quick 3 step process to performing Kegel exercises:
1. Identify the Pelvic Floor Muscles:
While urinating, stop the flow of urine midstream or squeeze the anus to stop from passing gas to locate the pelvic floor muscles. Only do this to help identify the proper muscles. In women, you're squeezing the muscles around your vagina. For men, you are focusing on the muscles in front of the anus. If your entire butt cheek is clenched down, you’re doing too much.
Now here’s a key point: Please don’t exercise the pelvic floor muscles while you are urinating! You should only stop your urine stream to identify the Kegel muscles for future exercise. It’s really not great for the bladder to stop your urine stream in the middle of emptying.
2. Contract and Relax:
There are a number of different Kegel muscle routines. To start, focus on squeezing the pelvic floor muscles for one second, then relax for one second. Repeat 10 times. Next set, perform a maximum contraction for up to 5 seconds. Don’t worry if initially you can only squeeze the muscles for 2-3 seconds. Then relax for 5 seconds. Again repeat up to 10 times.
3. Consistency is Key:
Similar to any other workout, developing a routine is essential. Perform these exercises regularly, ideally three times a day. Over time you will find that your strength is building and your symptoms of pelvic floor dysfunction are improving.
You should avoid performing Kegel exercises if you are suffering with symptoms of pelvic floor tightness such as:
- Constipation
- Pelvic pain including pain with intercourse, testicular pain, or
- Difficulty emptying your bladder
Kegel exercises will further tighten your pelvic floor muscles and may make your pelvic floor dysfunction worse.
Pelvic Floor Dysfunction Treatment
Non-Surgical Treatment Options for Pelvic Floor Dysfunction
Other than pelvic floor therapy and exercises, there are several other conservative options to treat pelvic floor dysfunction. What treatment option is best depends on your symptoms.
Medications for Pelvic Floor Dysfunction
Medications are most often prescribed to manage symptoms such as overactive bladder or pelvic pain. Be careful however when considering medications for these situations. If your overactive bladder symptoms are caused by constipation and poor bladder emptying (symptoms of a tight pelvic floor), then an overactive bladder medication can WORSEN your symptoms.
Pain medications for chronic pelvic pain should be used with caution. There is a serious concern for addiction if opioids are prescribed. It’s also possible that you will be masking the symptoms of something more serious or not treating the root cause of your pelvic floor dysfunction.
Pessaries For Pelvic Floor Laxity
Pessaries are devices which are inserted into the vagina to support pelvic organs in cases of prolapse. If you imagine the vagina is a room with 3 walls, and pelvic organ prolapse happens when one of the walls starts to cave in, then a pessary is a support beam to hold up the walls.
Pessaries are typically ring or donut-shaped and inserted in an office setting by a skilled practitioner. They are great for treating pelvic organ prolapse in women who are not sexually active or surgical candidates for a pelvic organ prolapse repair.
However, they can fall out if the prolapse is severe. They need to be changed and cleaned periodically to prevent infections or foul odors. This makes them less than ideal for women who are still sexually active.
Lifestyle Changes For Pelvic Floor Dysfunction
It’s amazing how often pelvic floor dysfunction, especially pelvic floor tightness, improves when you improve your lifestyle. A nutritious diet, regular exercise, consistent sleep for 8 hours, and stress management, should always be your top priority when treating any medical condition, including pelvic floor dysfunction.
Weight loss can often lessen the symptoms of urinary incontinence. A healthy diet rich in fiber is a great first step for constipation. Avoiding bladder irritants like caffeine, sugar, and alcohol will improve urinary symptoms from pelvic floor dysfunction.
Do not ignore the impact you can have on improving pelvic floor dysfunction when you focus on a healthy lifestyle.
Surgical Treatment Options for Pelvic Floor Dysfunction
Surgery should be the last option for pelvic floor dysfunction. Most symptoms can improve with conservative measures. However there are some select cases of pelvic floor dysfunction that require a more definitive surgical approach.
Pelvic Floor Reconstruction For Pelvic Organ Prolapse
When women have severe pelvic floor laxity leading to pelvic floor prolapse then it’s unlikely that conservative therapies are going to be sufficient. How do you know if your pelvic floor dysfunction is severe? If you feel a bulge extending out of the vagina and have to “push” your bladder or rectum back inside, then you may have severe pelvic organ prolapse.
Surgical repair of weakened or damaged pelvic floor muscles and tissues with or without a mesh can be safe and highly effective. Make sure you seek care from an experienced pelvic surgeon who performs routine prolapse repairs.
Urethral Slings and Bulking Agents for Stress Urinary Incontinence
Stress incontinence is a leakage of urine from coughing, sneezing, or straining. If you can’t jump on a trampoline or complete your Zumba class without urine leakage, then you have stress incontinence. This is often caused by a loosening of the pelvic floor muscles and tissues around the urethra.
Although pelvic physical therapy can be quite effective, you should consider surgery for stress urinary incontinence if your leakage:
- Has not improved with pelvic physical therapy.
- Is severe, requiring several incontinence pads a day.
- Bothers you enough that you want an immediate cure.
Several safe and effective surgeries exist for the treatment of stress urinary incontinence. Including mid-urethral slings and bulking agents like Bulkamid. Cure rates for these procedures range from 70-95% and they offer a quick recovery so you can get back to doing what you love.
Nerve Stimulation for Pelvic Floor Dysfunction
Although we have focused on the pelvic floor muscles, sometimes pelvic floor dysfunction is caused by nerve issues. There is a complex communication pathway between the pelvic floor, pelvic nerves, spinal cord and brain. If this pathway starts to dysfunction, then the pelvic floor muscles cannot function properly either.
Stimulation of the pelvic nerves can sometimes “rewire the circuitry” and improve pelvic floor dysfunction. Most nerve stimulators for bladder and bowel incontinence have temporary trial phases. In select cases where the pelvic floor dysfunction is improved, implantation of a permanent device can cure your symptoms.
Choosing the Right Treatment for Pelvic Floor Dyfunction
The choice of treatment depends on the severity of the dysfunction, patient preferences, and overall health. A thorough consultation with a healthcare provider specializing in pelvic health is essential for making an informed decision.
At Pazona MD Urology , we specialize in helping both men and women with pelvic floor dysfunction. Stop going to physicians who spend five minutes with you only to throw another antibiotic at your problem or say, “there’s nothing wrong with you.”
Get the care you deserve from our expert team who cares.
Conclusion
Pelvic floor health is crucial for overall well-being, affecting everything from continence to sexual function. Understanding the importance of pelvic floor muscles and recognizing the symptoms of pelvic floor dysfunction can lead to early diagnosis and effective treatment. Whether through pelvic floor therapy, physical therapy, or exercises, maintaining a healthy pelvic floor can significantly enhance quality of life. If you suspect you have pelvic floor dysfunction, consult a healthcare provider to explore your treatment options.
References:
https://my.instituteofphysicalart.com/media/ipa/pdf2/Laycock2001PERFECTscheme.pdf