When I attend a dinner party and meet someone for the first time, it inevitably leads to the following question: “So what do you do?” Before I answer, I try to read my audience.
In urology we have a lot of comic material because let’s be honest . . . I look at penises all day. If I don’t make myself and others laugh, we’d be questioning our sanity most of the time.
My G-rated answer is that I’m a urologist. Truthful and straightforward. People typically then respond to me in one of several ways:
1. Confused - “What is a urologist?”2. Disgusted - eyebrows raise as they think to themselves “Ewww . . . penises . . . gross.”3. Excitement, intrigued - smirk while they say out loud, “Can I ask you a question?”
I get it. Urology isn’t for everyone. But for some folks, this is their opportunity to ask the penis expert a question.
Let’s run through the more common questions to ask a urologist based on my personal experience. Most questions are asked in a professional office setting. Other times, I’m queried in line waiting for a cocktail.
Can you make “it” bigger?
No we cannot. If penis enlargement surgery were possible, Jeff Bezos would not be the richest man in the world. It would be a urologist.
Pretty much what you’re born with is what you got. Now here’s the good news. 90% of penises look about the same.
In a collection of 17 studies and over 15,000 the average erect penis length is about 5.16 inches. By their analysis, only 2% of men have penises longer than 7 inches, almost all of which have an internet side gig that is X-rated.
Some of you right now are probably feeling a little better about themselves. Here’s another confidence booster. With the aid of 3D models, women’s preferences for penis size came in slightly above normal at 6.3 inches. In other words, she doesn’t want you to be “King Schlong” either.
Let’s end on some good news. If you are obese, YOU can make “it” bigger with weight loss. Many men develop a buried penis as they pack on the pounds. Fat in the suprapubic area will conceal the length of the penis. Sometimes this requires surgery to remove, but in many cases, better food choices may be all you need.
Can you make me last longer?
Yes! Now we can help. I define premature ejaculation as reaching climax so quickly (< 2 minutes), that it causes you and/or your partner distress.
We are not certain why some men climax quickly and why others last 45+ minutes (these men are equally distressed and there’s no treatment to orgasm more quickly). In a study of over 500 couples demonstrated that the average length of a bedroom session is a whopping 5.4 minutes. This is probably a surprise given our new sense of what’s normal is being dictated by the online adult industry.
The therapies for premature ejaculation (PE) include:
- Condom usage
- Topical local anesthesia
- “Stop - start” method
- Oral medications
The most commonly used pills for PE are selective serotonin reuptake inhibitors (SSRIs), a class of antidepressants. When Prozac and similar drugs hit the market, a number of patients reported feeling better but started complaining of an ability to orgasm. The urology community said “Hey! We know some men who might like that side effect!”
SSRI’s for the treatment of PE are an off-label use (not what the medication was intended for treating). They work well, are well tolerated and safe in men without underlying depression etc. If you’re interested in learning more, you may want to consider a telemedicine visit with a PazonaMD urologist.
Can you make “it” work?
Erectile dysfunction (ED) is more common than you think. 50% of men by age 50 suffer with difficulty achieving or maintaining an erection. The incidence goes up 10% with every decade of life.
There are definitely ways to improve an erection. First it’s important to know how an erection occurs (don’t be a smart a$ here):
- Stimulation/interest (hormones)
- Nerves
- Blood vessels
80% of ED is due to atherosclerosis or blood flow issues. What causes this?
- Obesity (aka chalupas)
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
ED is also seen after pelvic surgery, radiation or trauma (nerve damage) or in men with low testosterone. An evaluation starts with a good history and some lab work. Next your doctor reviews the various treatment options including:
- Lifestyle changes
- Supplements
- Oral medications (e.g. sildenafil or Viagra)
- Vacuum erection devices
- Penile injections (ouch!)
- Penile prosthesis (really?!)
A detailed look at all of these topics is beyond the scope of this article. Here are the top 10 things you need to know from an ED doctor.
If you’re looking for a more personalized approach, set up a telemedicine visit with one of our ED experts.
Is bladder leakage normal?
Now that we’ve talked about penises, let’s shift gears for the rest of the audience and discuss your bladder. If there’s one thing you learn from this post it is:
BLADDER LEAKAGE IS NEVER NORMAL!
Too many women suffer in silence for no good reason. I guess it’s because grandma and mommy dearest were stoic, so you feel the need to do the same. No!
We can treat bladder leakage. A deep dive into all types of urinary incontinence is not our focus right now, but realize that we can help you if you have stress incontinence (coughing, laughing, sneezing), urge incontinence (“I didn't get there in time”), or both.
Treatments may include:
- Lifestyle changes (less coffee, more water)
- Oral medications
- Pelvic physical therapy
- Bladder conditioning devices
- Urethral slings
- Bladder Botox
- Sacral neuromodulation (bladder pacemaker)
The easiest way to get help is to have a telemedicine visit with the bladder expert.
How can I prevent kidney stones?
Kidney stones are miserable. At PazonaMD we believe prevention is the best medicine. If you’re looking for a deep dive on your DIY options to prevent birthing another rock baby from your pee tube, then check out our previous post on home remedies for kidney stones.
The Cliff Notes version of how to prevent a kidney stone is the following:
DRINK A LOT OF WATER EVERY DAY!
It’s not sexy, but water is effective. How much water? You want to aim for producing 2.5 L of urine a day. What goes in, must come out. If it’s summertime or you exercise a lot, then this may mean drinking > 3 L of water to make up for water loss through sweat.
More specific kidney stone prevention recommendations depend on your diet and how your kidneys filter minerals. Visit with a board-certified urologist, then they can order a 24 hour urine collection to investigate this further. You’ll receive a more personalized approach to preventing kidney stones.
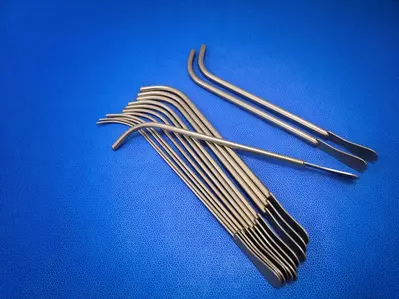
Do I need a stent after kidney stone surgery?
Not always.
If you’ve made it this far, then you probably are familiar with stents after kidney stone surgery. For the newbies, a stent is a necessary evil tool that keeps your kidneys draining after a kidney stone is removed surgically. They are evil because they can hurt as bad as the stone.
As a urologist determining whether to leave a stent or not is challenging. A blocked kidney due to swelling of the ureter is bad. Stent pain is bad as well. How do we decide on whether to leave a stent? Urologists look at several factors including:
- Size and location of the stone
- Length of surgery
- Amount of manipulation necessary to remove the stone
- Narrowing of the ureter
- Inability to remove all stone fragments
- Presence of an infection
If you do end up with a stent after kidney stone surgery, make certain you and your doctor are doing everything possible to minimize ureteral stent pain.
Will a vasectomy lower my testosterone levels?
No. Getting snipped does not mean you are going to lose any of your manliness. In fact, few things are sexier to a woman than a man who takes charge and removes the birth control responsibility off of her plate (this is closely followed by men who fold laundry).
The only job of the vas deferens, is to carry sperm from the testicle to where semen is produced (seminal vesicles). Testosterone is produced by the testicles as well, but then directly released into the bloodstream. A vasectomy will not impact testosterone levels.
The only thing a vasectomy lowers is the likelihood of you changing diapers 9 months from now.
Do I need a prostate exam?
At some point “YES”. Otherwise known as a digital rectal exam (finger in the butt), a prostate exam is a rite of passage for men as they deal with other joys of middle age; greying hair, losing hair, and growing hair in the wrong places.
To be clear, a urologist is not a butt doctor. We only go in the “exit only” area to feel the prostate for lumps that are concerning for prostate cancer.
Although prostate cancer screening guidelines are constantly changing, it’s a good idea to have your first prostate exam by age 50. Combined with an annual PSA blood test, this is the best way to make certain you don’t have prostate cancer.
Speaking of prostate cancer . . .
I heard most men die with and not from prostate cancer. Is this true?
Yes it is true. You’re more likely to die with prostate cancer than from prostate cancer. However over 30,000 men a year die from prostate cancer in the U.S. alone. Therefore burying your head in the sand and pretending that “prostate cancer won’t kill me” isn’t advisable either.
Although prostate cancer tends to be slow growing, and less aggressive, than many other cancers, it doesn’t mean that it can’t harm or kill you. Since it rarely causes symptoms until it’s too late, it is important to screen for prostate cancer before it becomes advanced.
Prostate cancer screening starts with an informed discussion between you and your doctor. If you elect to have a PSA blood test, and either your levels are high ( >4.0 ng/ml), or a prostate nodule is felt, then the next step is further testing. This may include an MRI, prostate biopsy or both.
If prostate cancer is diagnosed, then your urologist should spend a good deal of time with you reviewing the aggressiveness of your cancer and potential treatment options. Prostate cancer treatment is not a one-size fits all approach.
PazonaMD believes in patient education. If you or a loved one have been diagnosed with prostate cancer, and feel confused, scared or frustrated, then maybe it’s time for a second opinion with a PazonaMD specialist. We are here to guide you through this difficult decision-making process.
Why are you a urologist?
You’ve made it this far! Congratulations! Now for the question I am asked the most: “why are you a urologist.”
I have several creative answers, depending on my audience of course, however the simplest and most accurate is the following:
I help people pee and have sex. What is more noble than that?
I absolutely love my job. Now don’t get me wrong, I can do without insurance companies, fear of being sued, and unnecessary bureaucracy. But in terms of taking care of patients, I’m the luckiest guy around.
Practicing urology places me in a unique position to help you with some of your most important medical issues. Let’s face it, if you’re suffering with a kidney stone or UTI, you need help now. What’s more embarrassing than ED or bladder leakage? Don’t worry I can help.
Ultimately, PazonaMD was formed out of a desire to accelerate access to specialists like myself. We have a team of urologists ready to answer one of your questions. You can start your visit today.
If you have questions about whether a telemedicine visit is right for you, then feel free to call us instead: (615)527-4700.
Until then, I’m going to get back to work with my team of engineers. We’re sketching some plans for “making IT bigger” surgery . . . watch out Bezos.
(Disclaimer: PazonaMD is NOT actually designing any plans for a male enhancement surgery. Although this may be disappointing to some of you, our focus is on providing exceptional remote urology care.)